- Press Release – Don’t Miss Chacruna’s Psychedelic Culture Conference, March 29-30 - February 13, 2025
- Press Release – Enrolling Now: “Foundations of Plant Medicine Facilitation, Integration and Ethics” - August 23, 2024
- Will MDMA win FDA Approval? - August 2, 2024

Ali McGhee: Can you tell us a bit about you and your background?
NiCole T. Buchanan: I’m a Black woman from the United States, born and raised. I have a Ph.D. in Clinical Community Psychology from the University of Illinois Urbana-Champaign, and I’ve been a professor at Michigan State University for 22 years. I’m a licensed clinical psychologist and have trained with MAPS and CIIS, as well as Polaris for Ketamine. One of my main roles right now is the interim CEO and Board Chair for the Board of Psychedelic Medicine and Therapies.
AM: How did you become interested in psychedelics?
NB: My partner introduced me to the concept of using psychedelics for well-being around 2017. I feel like I was late to the party, but we came to it through more of a biohacking lens – through works about amplifying human ability, like Stealing Fire and The Rise of Superman. I got excited about the potential of psychedelics then.
What really changed things for me, as for so many people, was reading How to Change Your Mind. That was when I truly first began to understand the radical and transformative potential of using these to treat trauma. My area of clinical expertise is dealing with really complex trauma, and with the effects of multiple identities being targeted in your trauma. As people with multiple layers that’s what’s happened to us, we can experience harassment through both race and gender, for example. And if a person of color experiences interpersonal violence, they may also be dealing with race, and trauma around policing. And say they are assaulted by a loved one that is a man of color … I realized there is this amazing potential for these plant medicines to help heal trauma.
My area of clinical expertise is dealing with really complex trauma, and with the effects of multiple identities being targeted in your trauma.
I was working with a woman for a while who had made great progress but had so long to go before she could really experience wellness. I remember this rage bubbling up in me as I realized these plant medicines had been available methods of treatment a few decades ago, had been part of a lineage and legacy of healing for various populations, and had been intentionally taken away from us as a method of healing in the United States. I became committed to figure out how I could offer these when they became available.
My next real milestone was attending a 2019 MAPS training for clinicians of color. That was a transformative event – to be in a room with so many people that had their lineages and their own legacy of working with these medicines, and who worked with them as a spiritual healing process that connected with ancestor and source – that was my first time exposed to the depth and the beauty of that perspective, and the experience changed the trajectory of how I saw these medicines. In terms of what I wanted to be able to offer, I had thought of them in terms of the clinical or medical model. But the training opened my eyes to the potential of alternative healing models that could be used to transform all of society.
AM: I have heard that there was an evolution of these trainings to include more people of color and their perspectives – can you speak to that?
NB: I can’t speak to the conversations with MAPS that led them to believe diversifying the training was necessary. I know Monnica T. Williams was essential for pushing this to happen and getting donations to make it a possibility. I would hope that wasn’t the beginning of them having thoughts that we need more clinicians of color offering these services. I do believe there is increased awareness around this issue. Rick Doblin noted we are going to need “the 100,000” – 100,000 psychedelic-assisted therapists – to meet the need for these treatments once they become available. I’m not sure what estimates are based on, but looking at where the need is and how to create wellness beyond just healing, we need to make sure we have clinicians who represent the broad population. Right now, white people are primarily offering these treatments through clinical trials, and most people doing research are white too. There has not been enough to ensure people of color can access training to offer these services.
Beyond that, what is the infrastructure that needs to be created to put clinicians in place? For example, clinics need to submit documentation that they meet various specifications to offer this therapy, but what about the broader infrastructure? Do they have the right people in place? And the system currently benefits those working in clinical trials and highlights the medicalized model of these therapies. There is very little outside of those models to ensure people have access to information they need about what the infrastructure looks like. We need more information: what are the things that need to be checked off, and how do we get those done to open more clinics and serve people like us, to have clinicians that look like the populations they are serving?
Access to Doorways in the Oakland area (founded by Courtney Watson) is a wonderful model of a group of clinicians who identify as primarily queer, trans people of color offering ketamine-assisted therapy services for these populations in ways that are culturally sensitive. The center is set up specifically to meet the needs of BIPOC, LGBTQIA+ folks, and they are being very inclusive, up to making sure the clinicians also embody those identities and offer services in a way that is culturally responsive and informed. If we want to create a model to meet the needs of the diversity of our population, this is the type of offering we need to look at, not merely teaching people of color to offer the protocols in clinical trials – because that won’t be resonant for the population we serve.
In my clinic we don’t offer psychedelic-assisted treatments or ketamine-assisted therapy at this time, but I have been making sure to introduce clients to the idea that this is coming and will have great potential, not only for them but for others in their lives who are suffering. They will be able to say this medicine can be helpful, and maybe answer questions about the process.
Find more information on the upcoming Psychedelic Culture Conference.
AM: What are the special needs of POC when getting psychedelic therapy? What have you personally learnt about the needs of POC through your own training of becoming a psychedelic therapist?
NB: In my experience, there’s a lot of trepidation. And that makes a lot of sense if you have even a cursory knowledge of people of color in this country, including in medical trials and specifically with psychedelics. It’s really a frightening thing to ask people to willingly put themselves forward and subject themselves to this. Almost every community of color can identify medical abuses that have occurred because they trusted or had no power in the medical system. Whether they were denied treatment, or reports about things like Tuskegee were coming to Congress and no one raised the alarm. These people were put on a list, and all hospitals knew to deny them treatment.
Large systemic injustices and greed give people reason to be afraid and pause. It’s not paranoia. It’s a smart cultural mistrust.
Large systemic injustices and greed give people reason to be afraid and pause. It’s not paranoia. It’s a smart cultural mistrust. When we look at what’s happened with soldiers and prisoner populations forcibly enduring some of the most horrible tests, these are part of the stories that people are aware of and terrified of. White people have historically received mild to medium doses for white people in safe environments and experiences, while many black people have been imprisoned and shackled, and given heroic doses, 700-800 mcg of LSD, and left in a cell without consent or knowing what has happened to them. The legacies are very different in different communities, and people are legitimately terrified.
Then, with the legacy of the war on drugs and hyper police surveillance of communities of color, especially in poor black and brown comm, and the outrageous differences in sentencing for powdered versus crack rock cocaine, all of these things give people reason to be terrified to try to ingest drugs. As part of that legacy, many cultures have shared stories about someone who tried acid one time and never came back. We can try to interrogate that, but the stories exist and people believe them, and there’s enough truth in them to be afraid. We can’t academically explain to these communities that these are just fears. All of these, and a host more, are in the room when we are trying to convince people that this is a mechanism for healing and wellness. We have to be able to counter the legacy of rightful mistrust of medical and policing systems, where there has been a history of entrapment when people admit to drug use and are then incarcerated. And the ways people of color are surveilled by employers, other citizens, and police that would make them cautious about the idea of ingesting something that could flag them for a drug test. Without conversations about all of these issues, we will continue to leave certain groups out and won’t address the ways that they can have pathways towards access.
AM: Can you say more about what those pathways to access are and how they could be created?
NB: Number one: have a branch working to decriminalize or legalize the personal use of these substances, so that people can no longer be criminalized because of a trace amount in their system. If they have a personal use dose, ensuring they can use that and work in integration with a therapist, and that it can’t be something that will criminalize them.
Number two: a strong education campaign that is not just broad for everyone, but specific to various communities and the needs they have. If we want to be justice-focused, that needs to happen now. It cannot wait for all of these medicines to be approved for use, because by that time we will already see the disparities in place increasing. There will be whole sets of communities ready to go with education and without fear, and they will be first in line to get treatment and have these transformations. And other communities are on the periphery, without access. We can’t wait to share information to help these communities – and knowing the history it will be a lag of years. We have to do this work now if we want to help minimize disparities and access issues we know will be there. Who has insurance coverage and what is the quality? Who has access? If we are serious, we need to start addressing this now.

Discover the Indigenous Reciprocity Initiative of the Americas
AM: Can you tell me about your research in this particular field?
NB: I’ve been looking at barriers to equity and access as we move forward. My research is specific to the black community, but some concerns can be generalized beyond that. I’m trying to push the field to be thoughtful about what our biases are right now. Where do we stand in this moment, and what do we need to do to be better able to serve populations that deserve access? My fear is that, with the increase in commodification of these medicines and related procedures, we’re seeing a shift that’s now imminent: they will be approved. A lot of work is shifting towards the pieces that will be profitable. The risk we run there is that there will be less interest in this groundwork.
We need to embed justice and equity into our processes, and make sure organizations are focusing on access and equity. It’s always more difficult to try to retrofit these. If policy and protocol is created and we haven’t embedded them in equity or thought about inclusion concerns, we’ve embedded inequalities into the system that will exist for decades, and we’ve created systems that will need to be undone and dismantled. Often there is resistance to that and it’s more difficult. If we can slow down and embed these values into systems initially, there will be less to undo later, but the field will also have more success. If we want to see global healing, we can’t ignore the global majority and try to retrofit to their needs later. That has to be at the forefront to do this right.
If we want to see global healing, we can’t ignore the global majority and try to retrofit to their needs later. That has to be at the forefront to do this right.
Unfortunately, I see too many people in the field that don’t see why this should be a value. They believe that being a good human is enough. They don’t have enough understanding of the concerns people of color have to understand why the typical protocol is largely insufficient to address these needs. They believe this medicine has already healed them of sexism, racism, and homophobia. They have already arrived. That resistance is exactly what will fortify biases in and bolster inequities in these systems.
AM: Can you share a bit about Workplaces That Thrive, the training / education program you offer? What overlap do you see here between this and your work with psychedelic-assisted therapy and research?
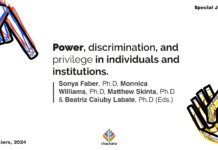
NB: One of the workshop series that I’ve been doing is looking at microaggressions and the way these show up every day in little ways in implicit biases. I’ve been doing these for the workplace for almost two decades, but the same concerns and issues exist in the psychedelics field. Bia [Labate] and I have an article in Chacruna that talks about responses people in the psychedelic community have to Black Lives Matter solidarity statements put out by some of the major psychedelic organizations. We saw some overt bigotry in the responses, as well as some of the more subtle or implicit biases of people not understanding why there’s an issue and thinking, “If we’re all just good people, it’ll go away,” or somehow thinking that talking about it creates racism.
As I mentioned, in the psychedelic space many people believe that because they have used these medicines, it has somehow cured them in all of the ways we are socialized to have biases. In any other context, we would know that’s ridiculous. Think about set and setting. You have to set your intention, and go in with a mindful intention, to address particular concerns. If you don’t, you’re just kind of doing molly at the club and not accessing healing. People who cannot say they deliberately went into a medicine session to address racism, homophobia, etc., come out feeling like they’ve elevated beyond internalized bigotry. The reality is that we’re all socialized in a space that gives us the same types of biases. We don’t have a medicine session that cures us and means we’re done with the work. If anything, it teaches us to engage in this work permanently, and highlights the ongoing need to engage.
People believing they no longer have work to do makes this an even more entrenched concern in psychedelic spaces. When I go into workplaces to do trainings, they expect that these biases are there. The way things have unfolded within the psychedelic world has been different. My favorite workshop is doing implicit bias work specifically for how biases show up in psychedelics.
I use vignettes based on real examples. So I’ll share a scenario, and ask, “What else might be going on here?” What often happens is that someone might understand one or two things on a surface level, but it’s rare for people to understand the real complexities around race, subjugation, and intergenerational trauma and how they show up. One thing I often see is clinicians not understanding the legacy of black people not really being able to swim. The issue is as recent as segregation and the defunding of public swimming pools, but we need to go back to looking at the trails of bones in the Atlantic. They threw people overboard because they couldn’t sustain their shipments – human beings. And the phrase “gator bait,” and what that actually looked like in the lives of real people. The terror of not being able to swim because it was an avenue for escaping slavery, the likelihood that black people have lost loved ones to drowning. It’s more than just telling someone to get a good cap to cover their hair. It’s steeped in generations of terror around water sources. While many people are aware of some of that and can talk about it, many don’t know the full depths of it, and white clinicians know almost nothing of that legacy and how it shows up today, what it means for people in the here and now. There can be an assumption that “my life experience translates into something meaningful for my client and me,” and they don’t realize they’ve just negated a pearson’s core experience in the world and proven i don’t have skill sets to provide care.

AM: How can white people be good allies to POC?
NB: I was just at an event where Courtney Watson [founder of Doorway Therapeutics] was talking about legacies of anger across groups of women of color. Someone brought up the same question, and her response was that when people tell you what they need, believe them. If money is a core need, people so often don’t want to help. People need to be ready to step up, or be honest that they’re not willing to step up in that way.
How do we create better equity for people to access trainings which is obscenely expensive and create clinics to serve the community when that process is also obscenely expensive? And how can we fund nonprofits for marginalized groups who have been historically overlooked?
Outside of funding these processes, people need to do their work. One thing Courtney said is, “If my anger upsets you it disturbs you, you have work to do. If you can’t hold the fact that I’m having strong emotions and that you upset me, and if you don’t understand what you did yet and your response is to tell me how I’m wrong and shouldn’t be upset, that’s an indication that you’re not doing the work.” And these responses mean that you’re not doing the work you need to do to offer services for these populations.
We need folks to get trained up, because there are simply not enough providers. If white providers could effectively do this kind of work across racial differences, understand the nuances of race, gender, class, and sexuality, and have rich conversations and know history to understand comments and not give silly flippant responses, then we are in a place where we can see radical transformation happening. It’s not to say, “Stay in your silo and don’t do this work with people of color,” it’s actually, “Accelerate your training on this issue specifically because you are desperately needed.” Many people of color will need to work with people of color to do their work for healing, and they could benefit from chunks of that work happening with a white therapist who has done their own work, and who can sit and hear through pain and be present as a witness. That could be healing in a vastly different way. We will have to break down these silos to work together, and to come from a space of being thoughtful and conscious.

Shop our Collection of Psychedelic T-Shirts.
AM: Can you speak about your work with the Board of Psychedelic Medicine and Therapies?
NB: We are on the verge of seeing that future where psychedelic therapies are widely available. We are even quickly approaching where some of these treatments will be covered by insurance. It’s a glorious time we’re about to enter, but we have a lot of work to do to ensure the public can turn to our field and feel they can trust what we are doing.
That question: “Can I trust that I can go to someone for this treatment and be in safe care?” That is the work of the Board of Psychedelic Medicine and Therapies. We are creating a credentialing process to determine who is knowledgeable and who has the appropriate training to offer these treatments for the general public, so that someone can expect safe spaces where they will be safe and have appropriate care. This is a critical piece of work for the field. If we can’t establish that our care providers have the appropriate training and knowledge, we will lose the trust of the public, and our field will pay the price.
The board is working to create the credentialing process so that people who are already in a licensable profession can demonstrate that they are certified to offer this treatment.
Creating a more equitable process in psychedelics means we don’t only have a process for clinical or research practice, but also for our legacy and lineage practitioners.
But, going back to what I said earlier, if we only focus on credentialing those in a licensable profession, we are only focusing on those who need to heal because there is something diagnosable for them. The ones insurance will cover will have expanded access, but the goal isn’t merely taking us from illness to healing. I want to see the entire community go beyond that into wellness, which means we have to have pathways for those who don’t fit or don’t want a medical model. Perhaps they don’t have a diagnosable condition; they want a ceremonial or spiritual practice and not a medical practice. That’s more complicated, but we want to create pathways for our lineage and legacy practitioners, those practicing in what’s often termed the underground. We want them to have space in the field and be visible. There is expertise outside of medicalized expertise. Creating a more equitable process in psychedelics means we don’t only have a process for clinical or research practice, but also for our legacy and lineage practitioners. The lineage and legacy pathway is infinitely more complicated, and we need to make sure when we’re doing this that it’s safe and legal for them to come forward, but we want to also ensure there’s a pathway for these practitioners to work legally and safely as well.
Art by Trey Brasher.
Take a minute to browse our stock:
Did you enjoy reading this article?
Please support Chacruna's work by donating to us. We are an independent organization and we offer free education and advocacy for psychedelic plant medicines. We are a team of dedicated volunteers!
Can you help Chacruna advance cultural understanding around these substances?